
A hysteroscopy with endometrial curettage is a common procedure can be done as an outpatient procedure or a day case procedure under general anaesthetic. This is done to examine and treat conditions within the womb. A hysteroscope—a slim telescope with a camera—is inserted through the cervix to allow direct visualisation of the uterine cavity. This is combined with curettage, where the lining of the womb (endometrium) is gently removed with a small instrument or suction. The procedure is often performed for women with abnormal uterine bleeding, post-menopausal bleeding, suspected uterine polyps or fibroids, recurrent miscarriage, or thickened endometrium. It may also be carried out when other investigations have shown irregularities. As a minimally invasive daycase procedure, hysteroscopy and curettage avoids the need for overnight hospital stay. It is performed under short general anaesthesia, typically taking less than 30 minutes, and provides diagnostic clarity.
Recovery after hysteroscopy with curettage is usually straightforward. Patients may experience mild cramping, spotting, or light bleeding for a few days. Most women resume normal activities within 24–48 hours, although strenuous exercise and sexual activity should be avoided until bleeding stops. The tissue removed is sent for testing to check for hyperplasia, fibroids, polyps, or cancerous/pre-cancerous changes. Results are usually available within next few weeks. Risks are very low but may include bleeding, infection, and uterine perforation. A polyp or submucous fibroid resection with Myosure can be organized at the same time.

The MyoSure procedure is a minimally invasive technique used to remove polyps and small fibroids inside the womb. These growths often cause heavy bleeding, pain, or fertility problems. A slender instrument is introduced via a hysteroscope, allowing precise removal of the abnormal tissue while preserving the womb lining. The procedure takes less than 30 minutes under sedation or anaesthesia. As there are no incisions, recovery is rapid and women usually return home the same day.
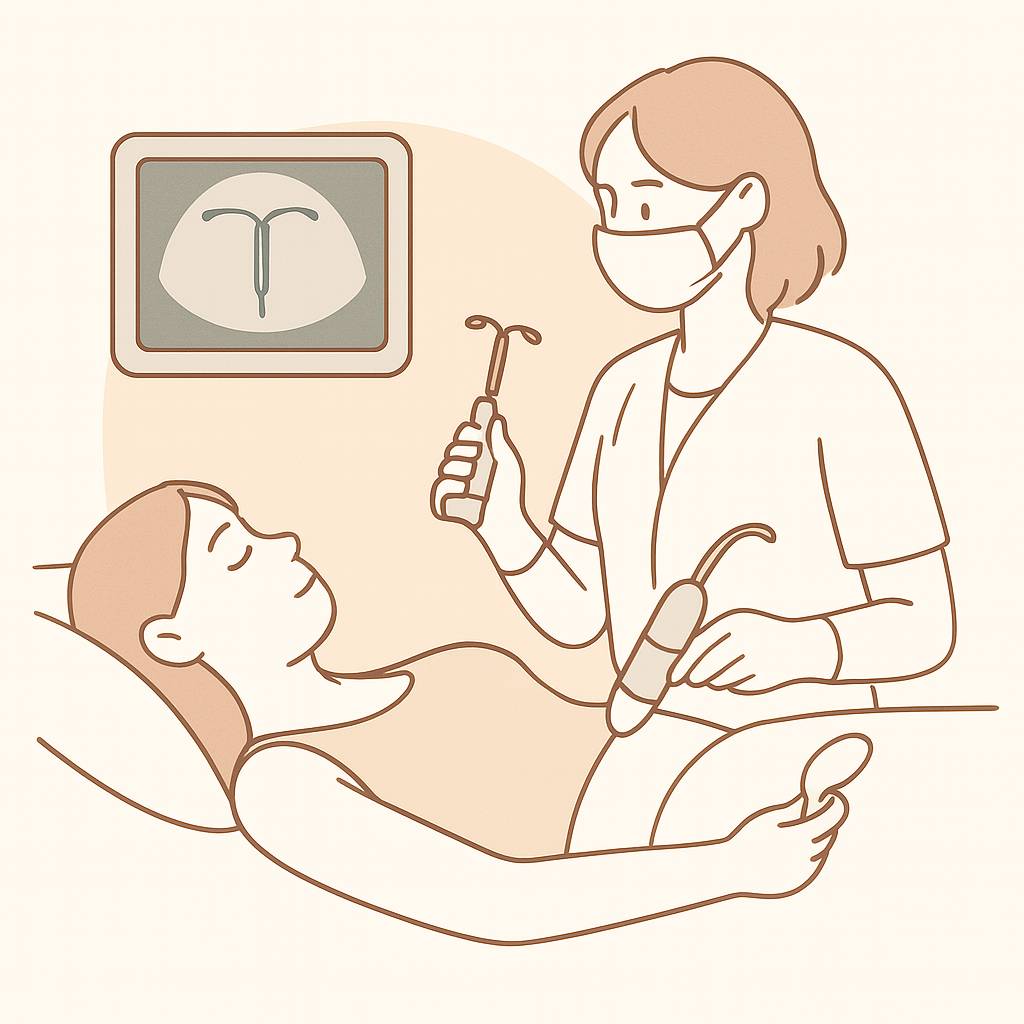
The Mirena intrauterine system (IUS) is a small device fitted into the womb to provide long-term contraception and treatment for heavy bleeding. While usually inserted in the clinic, some women require insertion, removal, or replacement under anaesthesia due to anxiety, pain, or complex anatomy. Under sedation or light general anaesthesia, the procedure is performed comfortably and safely as a daycase. The Mirena provides highly effective contraception for up to 8 years and is also used in treating heavy menstrual bleeding, endometriosis, adenomyosis, and as part of hormone replacement therapy (HRT). Removal or replacement under anaesthesia may also be needed if the strings are not visible or if the coil has become embedded.

Endometrial ablation is a minimally invasive treatment for heavy periods where the womb lining is destroyed using heat, radiofrequency, or other techniques. It is ideal for women who have completed their families and want to avoid hysterectomy. The procedure takes as a daycase, under general anaesthesia. It dramatically reduces menstrual flow, and in many cases, periods stop completely. Ablation provides a relief from symptoms without the need for open surgery.
Recovery is usually quick, with women resuming light activities within 24–48 hours. Some discharge and cramping may occur for a few days. Risks are rare but may include infection or uterine perforation. Pregnancy after ablation is unsafe, so contraception is advised. Our clinic ensures careful selection of suitable candidates, expert surgical practice, and comprehensive follow-up. Endometrial ablation provides a safe and effective alternative to hysterectomy, improving quality of life for women with heavy bleeding.

Laparoscopy, or keyhole surgery, uses a camera inserted through the belly button to diagnose and treat pelvic conditions. It is recommended for pelvic pain, suspected endometriosis, or ovarian cysts. The procedure allows direct visualisation of the womb, ovaries, and fallopian tubes, with therapeutic interventions such as cyst removal or adhesiolysis often performed at the same time. As a minimally invasive approach, laparoscopy offers quicker recovery, less pain, and smaller scars compared to open surgery.
Recovery is fast, with most women discharged the same day. Light activities resume within a few days, and full recovery usually occurs within 2–4 weeks. Risks are low but include infection or injury to nearby organs. We provide these with modern technology, providing a safe and effective way to both diagnose and treat gynaecological conditions in one procedure.

Laparoscopic salpingectomy (removal of fallopian tubes) or oophorectomy (removal of ovaries) is performed for conditions such as ovarian cysts, endometriosis, cancer risk reduction. Through small incisions, a camera and instruments allow precise removal while minimising trauma. This minimally invasive approach offers shorter hospital stays, reduced pain, and quicker recovery compared to open surgery.
Recovery is usually within 2–4 weeks. If one ovary remains, fertility and hormone production may continue. Removal of both ovaries causes surgical menopause, for which HRT may be advised. Risks are rare but include bleeding, infection, or injury to nearby structures.

Ovarian cystectomy involves removing cysts while preserving healthy ovarian tissue. It is commonly recommended for women with persistent, large, or symptomatic cysts. Using keyhole incisions, the surgeon carefully excises the cyst while protecting ovarian function, making it ideal for women wishing to preserve fertility.
Recovery is quick, with most women returning to normal activities within few weeks. Risks are low but include recurrence or rare complications.

A Total Laparoscopic Hysterectomy (TLH) removes the uterus through keyhole incisions. It is performed for fibroids up to 3-4 cms in our set up, endometriosis, adenomyosis, abnormal bleeding. Compared with open surgery, TLH offers smaller scars, less pain, reduced blood loss, and faster recovery, making it the preferred option for many women.
Most women leave hospital within 24–48 hours and recover within 4–6 weeks. Risks are low but include infection or injury to nearby organs.

A Total Abdominal Hysterectomy (TAH) removes the uterus through an abdominal incision. It is recommended for large fibroids, bulky adenomyotic uterus when keyhole surgery is not suitable. Although recovery is longer, TAH provides a definitive solution, relieving symptoms and improving quality of life.
Recovery usually takes 6–8 weeks, with a hospital stay of 2-3 days. If ovaries are also removed, surgical menopause occurs, for which HRT may be discussed.

Myomectomy removes fibroids from the uterus while preserving fertility. It is recommended for women with heavy bleeding, pain, or infertility linked to fibroids. When fibroids are large or multiple, an open abdominal approach may be needed. This surgery allows women to retain their uterus, offering hope for future pregnancies.
Recovery is usually 6–8 weeks, with significant improvement in symptoms once healed. Risks include bleeding or adhesions, but benefits include restored fertility and lighter, more regular periods.

When fibroids grow very large, they can enlarge the uterus significantly, causing heavy bleeding, pain, and pressure. In such cases, open surgery may be required, either myomectomy (fibroid removal) or hysterectomy, depending on fertility wishes. Open surgery allows safe removal of very large fibroids.
Recovery usually takes 6–8 weeks, with improved quality of life once healed. Risks are slightly higher due to distorted anatomy.